Hormones in Male Reproductive System
The function of the male reproductive system depends on the action of several chemicals and hormones that are produced by different body glands. Some of these hormones are named as tropic hormones due to their ability to launch other hormones. Other hormones of the male reproductive system have a direct relation to body systems and organs while controlling the production of semen and range of emotions. Note that, the male reproductive system does not follow hormone fluctuation cycle per month like females rather these hormones stay consistently active in the body throughout their life.
There are five major types of hormones in the male reproductive system; essential details about these fluids are discussed as below.
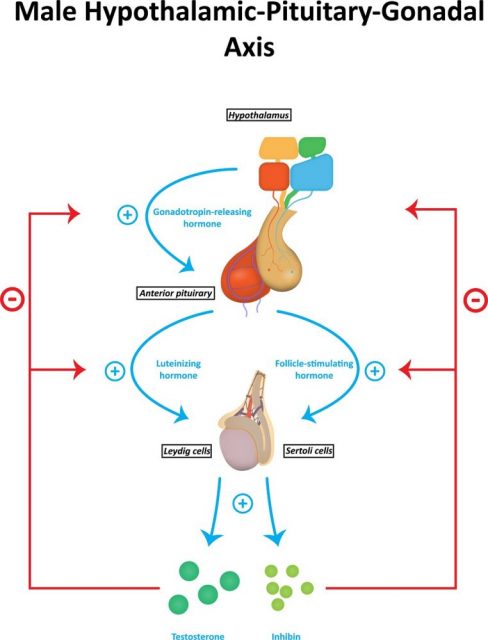
Gonadotrophin-Releasing Hormone
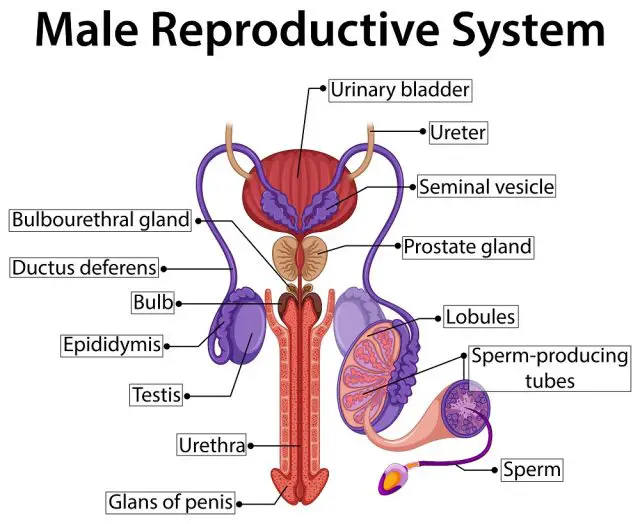
This hormone is secreted and produced by specialized nerve cells in the brain hypothalamus. The released fluid flows to pituitary glands through tiny blood vessels and then stimulates two new hormones named as a luteinizing and follicle stimulating hormone. These hormones are further released to complete general circulation in the reproductive system, and they work on testes to manage various functions of the reproductive system. Luteinising and follicle stimulating hormones also control the production of sperm in the male reproductive system.
- Facts behind the production of Gonadotrophin-releasing hormone:
The Gonadotrophin-releasing hormone levels are quite low in children, but as the person approaches puberty stage, the production automatically increases. It ultimately triggers sexual maturation in males. Note that, when testes become completely functional, the production of follicle stimulating hormone, luteinizing hormone, and gonadotropin-releasing hormone are controlled by testosterone in males. Studies reveal that if production of testosterone rises, it leaves an inverse impact on Gonadotrophin-releasing hormone leading to its decay in the reproductive system.
- Having too much Gonadotrophin-releasing hormone:
There are rare studies that provide exact information related to effects associated with the too much Gonadotrophin-releasing hormone. In some extreme cases, pituitary adenomas, a kind of tumor can develop that cause overproduction of testosterone.
- Having too less Gonadotrophin-releasing hormone:
Some children face a deficiency of Gonadotrophin-releasing hormone in the growth stage that clearly means their reproductive system is not ready for the puberty. Few cases of Kallmann’s Syndrome, a rare genetic disorder, is also reported that causes loss of production of Gonadotrophin-releasing hormone while interfering with sexual maturation and pubertal development. This improper development of testes may also cause infertility.
Follicle Stimulating Hormone
As already discussed, stimulating follicle hormone is also one of the gonadotrophin-releasing hormones that are produced in combination with the luteinizing hormone. This hormone is released into the male body by pituitary bland and flows via the bloodstream. This hormone plays an essential role in pubertal development as well as male testes. Experts reveal that stimulating follicle hormone works like Sertoli cells in testes and it helps to boost production of sperms.
- Facts behind the production of stimulating follicle hormone:
The production of stimulating follicle hormone is controlled by various circulating hormones present in testes. This system is well known as a hypothalamic-pituitary-gonadal axis. When a gonadotrophin-releasing hormone binds to receptors in the anterior pituitary gland, it stimulates the production of follicle stimulating hormone along with luteinizing hormone that is further carried to testes via the bloodstream. This hormone plays an essential role to control various functions of testes in a male body.
Production of follicle stimulating hormone in men is controlled by testosterone and inhibin; note that both of these hormones are produced in testes. The fixed cycle in male reproductive system regulates testosterone levels as per availability of stimulating follicle hormones. The rise of testosterone is observed by nerve cells present in the hypothalamus that further decreases the production of the gonadotropin-releasing hormone, directly reducing production of stimulating follicle hormone and vice versa. This process is termed as negative feedback control, and it helps to maintain steady levels of testosterone in the body.
- Having too much follicle stimulating hormone:
Higher levels of follicle stimulating hormone in men indicate malfunctioning of testes. When gonads are not able to develop enough amount of testosterone or inhibin, the feedback control is lost, and level of follicle stimulating hormone rises. This state is known as hypogonadotropic-hypogonadism that further leads to failure of the testicular system. This condition in the male reproductive system is named as Klinefelter’s syndrome.
- Having too less follicle stimulating hormone:
Sufficient production of stimulating follicle hormone is essential for appropriate sperm development in the male reproductive system. If a man suffers from the complete absence of stimulating follicle hormone, it may cause lack of puberty, or in worst cases, it leads to infertility. Partial deficiency of follicle stimulating hormone in male causes delay in achieving a state of puberty due to limited sperm production; however, it doesn’t cause much interference in fertility. In case if someone suffers the loss of follicle stimulating hormone after achieving puberty stage, it may also cause infertility.
Luteinizing Hormone
Same as stimulating follicle hormone, luteinizing hormone is also a gonadotrophic releasing hormone that is developed in anterior pituitary glands. This hormone is also responsible for regulating operation and function of testes. In the male reproductive system, luteinizing hormone assists in stimulation of Leydig cells that further leads to the production of testosterone in testes; this hormone provides support for sperm development.
- Facts behind the production of luteinizing hormone:
The process of production of luteinizing hormone is same as follicle stimulating hormones as discussed earlier. Note that the secretion of hormones from gonads causes suppression of production of a gonadotrophic releasing hormone that further reduces the development of luteinizing hormone in anterior pituitary glands. The moment when hormone production in gonads falls, it triggers the reverse process by increasing the production of gonadotrophic releasing hormones while boosting secretion of the luteinizing hormone as well. In simple words, this control mechanism also works on the basis of negative feedback. Medical health reports reveal that it is important to maintain fine-tuning of luteinizing hormone because it has a direct impact on fertility.
- Having too much luteinizing hormone:
The rise of luteinizing hormone in the male reproductive system leads to infertility. As production and release of luteinizing hormone are completely maintained by hypothalamic-pituitary-gonadal axis, a higher amount of this hormone in the bloodstream can decay the production of sex steroid in testes. Having too much luteinizing hormone can also cause some adverse genetic conditions such as Klinefelter’s syndrome in which male reproductive system carries one extra X chromosome leading to the formation of XXY instead of XY. Hence, the small testes are not able to support appropriate secretion of testosterone causing improper sperm development.
- Having too less luteinizing hormone:
Too little production of luteinizing hormone is also a common cause behind infertility in men because a set level of luteinizing hormone is essential to allow normal functioning of testicular. Low level of luteinizing hormone in the male reproductive system can cause Kallmann’s syndrome that is related to the decay in the secretion of a gonadotrophin-releasing hormone in the hypothalamus.
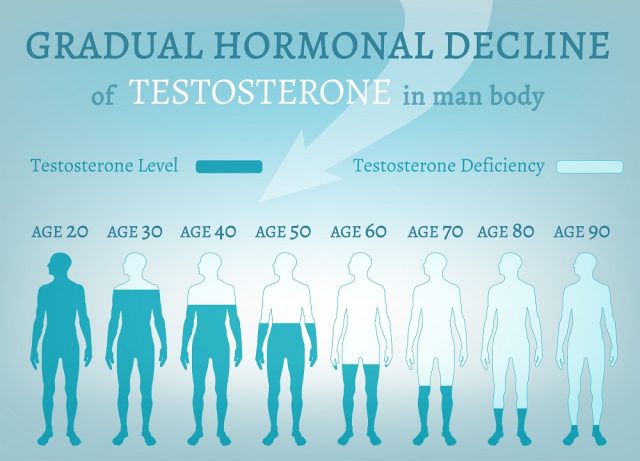
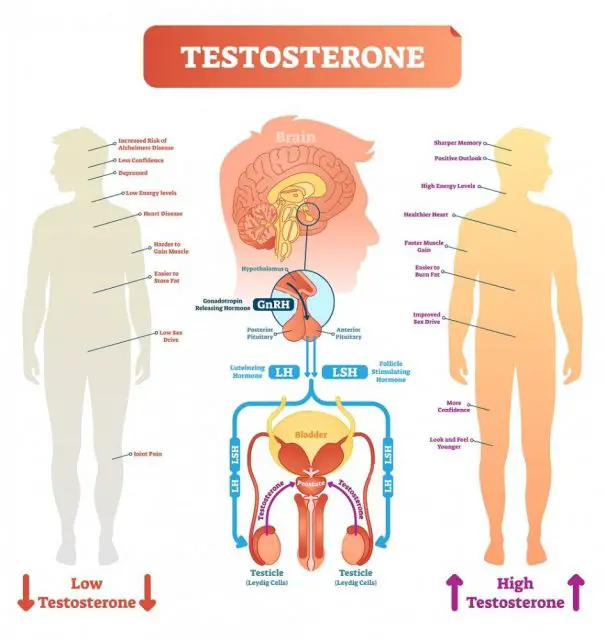
Testosterone Hormone
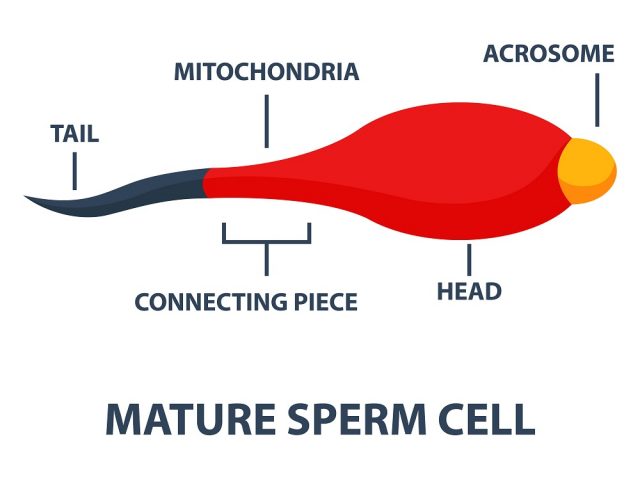
Testosterone hormone is produced by Leydig cells in testes; however, a small amount of this hormone is also secreted by adrenal glands. During fetal development, testosterone is responsible for the production of internal and external reproductive systems in men; it also plays an important role in the secretion of sperm in adults. Testosterone hormone stimulates the body to generate new blood cells so that bones and muscles can become able to handle the puberty stage while maintaining appropriate libido level in the body. Medical health experts say that Testosterone hormone is responsible for several changes in the human body including the growth of pubic hair, body hair, increase in height, penis enlargement, development of testes gland and changes in sexual behavior. This hormone also controls the production of stimulating follicle hormone and luteinizing hormones. In order to regulate all changes in the body, testosterone is often converted into androgen that is named as dihydrotestosterone.
- Facts behind the production of testosterone hormone:
Testosterone levels are highest in the body during morning hours and start decaying after that. The amount of Testosterone hormone produced in testes is controlled by pituitary gland and hypothalamus. Note that pituitary gland releases luteinizing hormone with respect to the production of gonadotropin-releasing hormone. Luteinising hormone further travels to gonads via the bloodstream, and there is stimulates the production of testosterone. As the testosterone amount increases in blood, it sends feedback to suppress gonadotrophin releasing a hormone in the hypothalamus that further suppresses the development of luteinizing hormone in the pituitary gland. As a result, in response to this negative control feedback, the testosterone levels start falling again.
- Having too much testosterone hormone:
The impact of the excessive production of Testosterone hormone completely depends upon the age of the person. There are no reported cases of any side effect of too much Testosterone hormone in adults; however, the presence of higher level of testosterone in young children may cause false growth if spurt while leading to early puberty. Experts say that too much production of Testosterone hormone in males can also cause precocious puberty that is the major cause of infertility.
- Having too less testosterone hormone:
In case if a deficiency of Testosterone hormone is observed during the fetal development stage of man, it may cause improper growth of male characteristics. When Testosterone hormone deficiency occurs in puberty stage, the boy may suffer troubles in normal growth and had no growth for a spurt. Lesser amount of Testosterone hormone in child leads to the lesser growth of pubic hair, penis and improper deepening of the voice. Boys having lesser Testosterone hormone in their reproductive system also have lesser endurance and strength. Note that, Testosterone hormone growth decays with age that this state is known as male menopause.
Inhibin
This hormone is produced by cells present in testes, and it is responsible for monitoring overall health and maturation of sperms in the male reproductive system. It is generally produced by corpus luteum, placenta, pituitary gland and gonads. Although it is produced by several tissues, still gonad is considered a major site for secretion of inhibin. There are two types of inhibin hormones that are secreted from gonads; they are inhibin-A and inhibin-B. Inhibin in the male reproductive system is also responsible for regulating the production of embryonic, gametes and fetal development. This hormone is produced by testes, and it travels to the brain via bloodstream where it helps to control the secretion of the gonadotropin-releasing hormone. With decay in the production of the gonadotropin-releasing hormone, level of luteinizing hormone and follicle stimulating hormones also fall; it further slows down the sperm production.